More ways than ever...
Today there are more tools than ever to prevent HIV. Strategies include using condoms, not sharing injection equipment, and taking a daily pill to prevent HIV (PrEP). Getting tested and treated for STDs can lower your chances of getting HIV. Not having sex and not injecting drugs ensure that you won’t get HIV.
Treatment is Prevention! People living with HIV who stay on their medication and have so little virus in their body that a blood test cannot measure it, don't give HIV to a partner through sex. The Centers for Disease Control and Prevention indicate there is strong evidence about treatment as prevention for other ways HIV can be transmitted, but more research is needed for other ways, including breastfeeding and injection drug use.
Getting tested is the first step in getting on PrEP if you are HIV negative. Getting tested is also the first step in getting medical care to become virally suppressed if you are HIV positive.
Abstinence
While there have been many strides in HIV prevention tools, abstinence is still the only 100% method to prevent HIV and other sexually transmitted diseases (STDs). The longer you wait to have oral, vaginal, or anal sex, the fewer sexual partners you are likely to have in your lifetime. Having fewer partners lowers your risk of encountering a partner who has HIV or an STD.
 Condoms
Condoms
If used correctly condoms are highly effective in preventing HIV and some STDs. Condoms do not provide good protection against STDs that are transmitted through skin-to-skin contact. Gonorrhea and chlamydia are two examples.
There are two types of condoms: male and internal (also known as female). It is important that you know how to use both correctly for your protection.
For both male and internal condoms, only one condom should be used at a time. Using multiple condoms at one time increases friction and the likelihood that both condoms would tear.
A new condom should be used each time a sexual encounter occurs. After a condom is used it should be properly disposed of.
Even if condoms are used the right way every time you have sex, there is still a chance of getting HIV or STDs. For some individuals at high risk of getting or transmitting HIV or STDs, adding other prevention methods may be ideal.
-
Need Condoms?
Looking for a place near you to grab some free condoms? All local health departments have free condoms. Most community agencies that provide HIV testing offer free condoms. Click "Find Condoms" then use the HIV & STI Testing button.
Male (External) Condoms
A male condom, also called an external condom, is a thin layer of protection that is worn over the penis during sex. It is available in different materials.
- Condoms made of latex provide the best protection against HIV and STDs.
- Polyurethane (plastic) condoms are a good option for those with latex allergies. However, they break more often than latex condoms.
- Natural membrane condoms (such as lambskin) have small holes in them. They DO NOT protect against STDs or HIV.
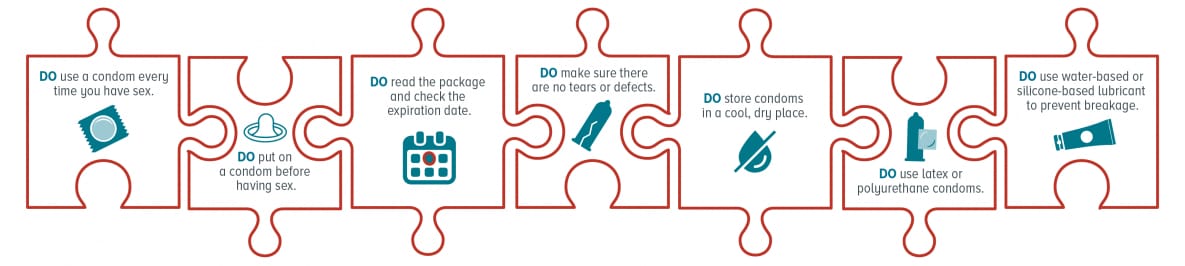
- Male (external) condoms do’s and don’ts
Internal Condoms
Internal (or female condoms) are thin pouches made of a thin latex product called nitrile. It can be inserted into the vagina or anus for intercourse.
- The internal condom can be inserted up to eight hours before intercourse.
- For vaginal sex, the inner ring should be squeezed. With the inner ring squeezed, put the inner ring and pouch inside of the vagina. After sex, twist the outer ring and carefully pull gently to remove the condom.
- For anal sex, the inner ring should be removed before insertion.
Lubrication
Lubrication, or lube, assists with HIV and STD prevention. It can help prevent condoms from breaking and slipping. Water-based and silicone-based lube is safe to use with all condoms.
- Oil-based lubes and products containing oils (including hand lotions, Vaseline, and Crisco) should not be used with latex condoms. They can break down the latex and cause the condom to break.
- It is safe to use any type of lubricant with internal/female condoms as they are made of nitrile.
- Lubricants containing nonoxynol-9 should not be used as it can irritate the lining of the vagina and anus. The irritation can increase the risk of HIV or STD infection.
The Right Way to Use a Male (External) Condom
Medication
There are currently several strategies to prevent HIV with medication. If you are at risk for contracting HIV, you may take a pill daily prior to any risk behaviors. This is called HIV pre-exposure prophylaxis (PrEP). If you have already potentially been exposed to HIV, you may also take medication to prevent infection. This is called post-exposure prophylaxis (PEP). If the exposure is non-occupational it is called nPEP. PEP and nPEP must be administered within 72 hours of a potential exposure. For more information on PrEP or nPEP, visit our PrEP and nPEP page.
Additionally, it has been proven that persons living with HIV that are on their HIV medication, and have a low number of copies of virus in their system will not transmit the virus to their HIV-negative partners sexually. This is called treatment as prevention, or TasP. For more information on TasP, visit CDC.gov.
Comprehensive Harm Reduction
People who share needles, syringes or other equipment to inject drugs, silicone or hormones are at high risk for getting HIV, hepatitis A, hepatitis B and hepatitis C. Reusing needles can also lead to infections such as skin abscesses and endocarditis (a heart infection). Comprehensive Harm Reduction programs (also called needle exchange or syringe services) help people reduce the negative health impacts of drug use. These programs provide new syringes and needles, disposal of used syringes, referral to drug treatment and medical care, Naloxone (to reverse overdoses), education and counseling, testing for HIV, hepatitis and other diseases, and referral to social services and insurance. Location of Comprehensive Harm Reduction programs in Virginia can be found on our CHR page.
Expecting Mothers
If you are pregnant it is very important to talk to your healthcare provider.
If you are unaware of your HIV status it is important to get tested and follow the recommendations of your provider. These recommendations could include preventative methods such as PrEP if your partner is HIV-positive.
Mothers that are HIV-positive should follow recommendations from their provider and make sure that they take their medications as prescribed. If you are treated for HIV early in your pregnancy the risk of transmitting HIV to your baby can be 1% or less. Breast milk contains HIV. Even with an undetectable viral load breastfeeding should be avoided.

