Download a pdf version of this document
By Michael Landen, MD, MPH & Helen Tazelaar
COVID-19 Health and Disease Disparities by Race and Ethnicity in Virginia
Racial and ethnic health disparities illuminate areas where significant health and disease inequity exists. Unfortunately these disparities exist far too often in the United States and Virginia, and this is no different for key measures of the COVID-19 pandemic. Disparities in COVID-19 case, death and vaccination rates have been demonstrated in the United States and have been particularly unfavorable to Hispanic and Black populations. Life expectancy in the United States is projected to be reduced at least 3 times more for Hispanic and Black populations than for White populations as a result of COVID-19, wiping out ten years of progress in bridging the life expectancy gap between White and Black Americans. But opportunities exist as there is both an abundance of data being collected about and resources being directed to addressing COVID-19 and its complications. By recognizing these disparities and prioritizing strategies to address them, overall population health and that of the most at-risk subpopulations can be improved.
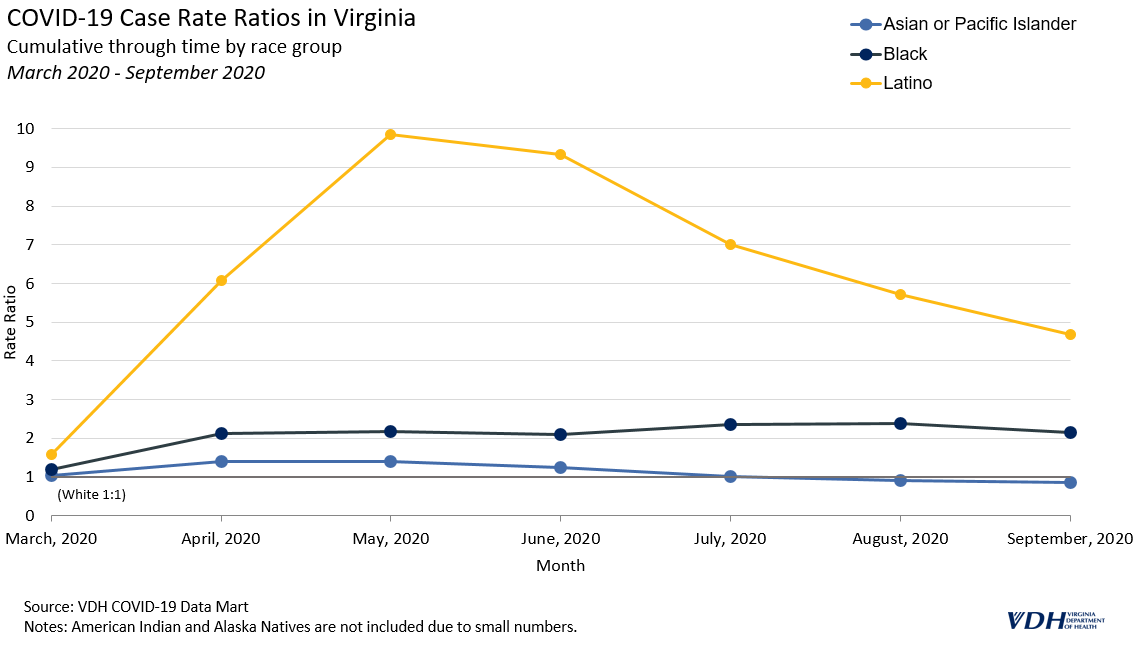
COVID-19 Cases
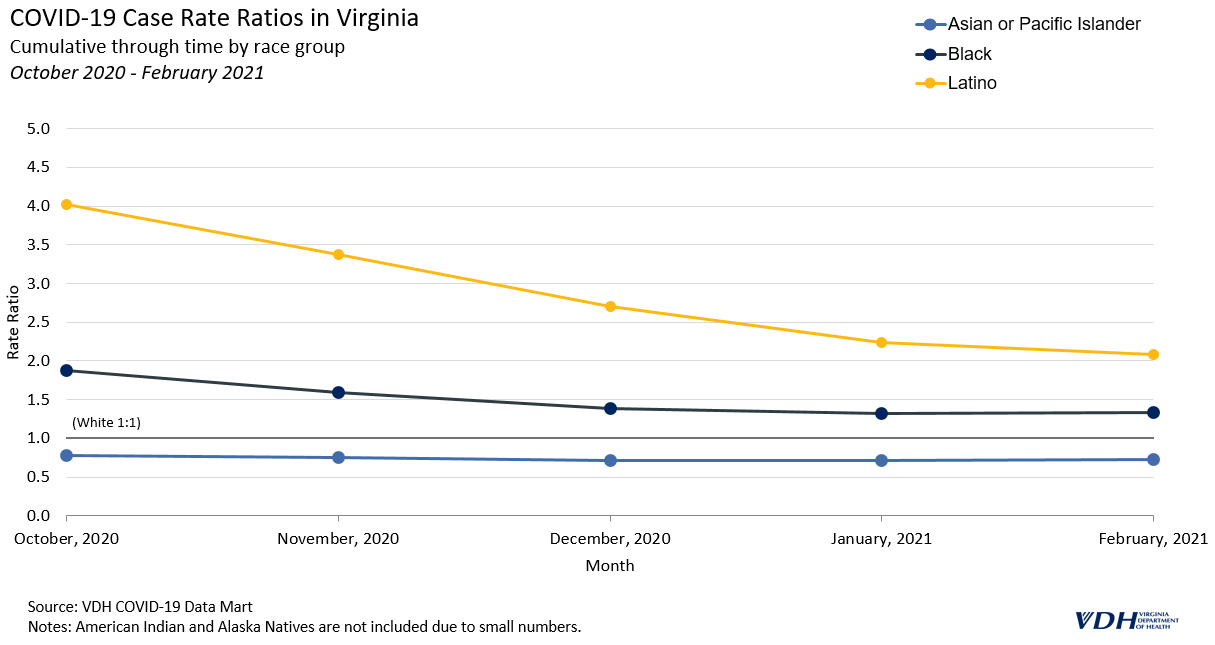
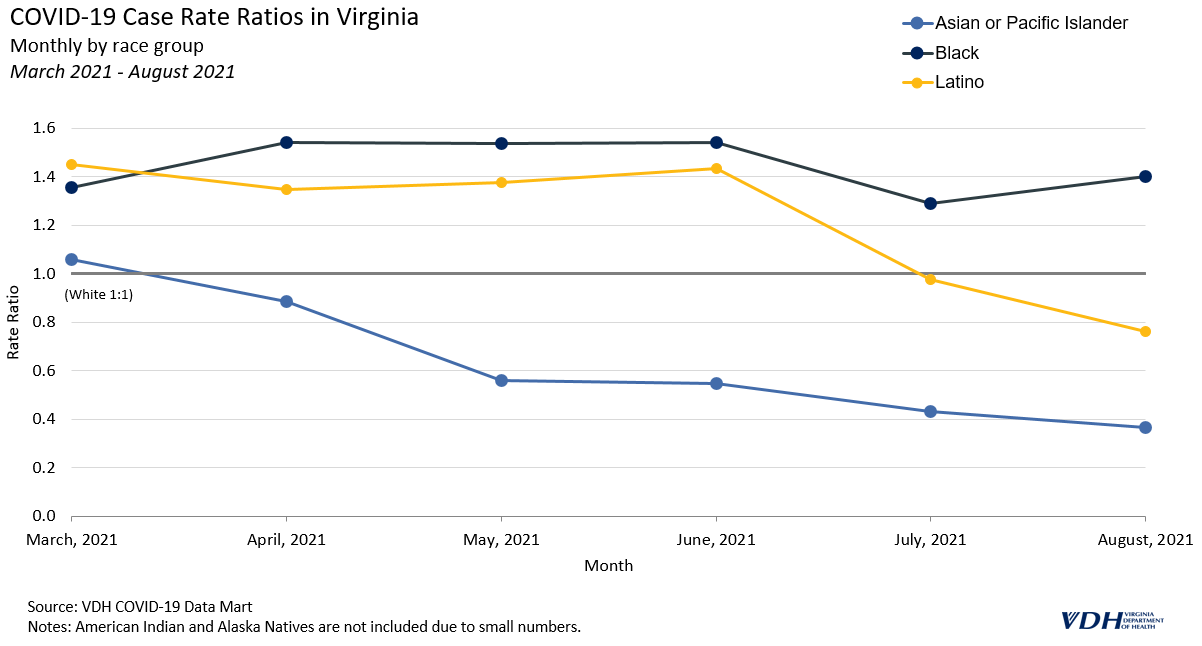
COVID-19 case rates in Virginia are substantially higher for Hispanic and Black populations than for other racial/ethnic groups. When compared to the White case rate, the Black case rate is 1.3 times higher and the Hispanic rate is 2.1 times higher. The Asian and Pacific Islander population has the lowest case rate at 0.7 times that of the White population.
COVID-19 Hospitalizations
COVID-19 hospitalization rates are also higher for the Hispanic and Black populations than for other racial and ethnic groups. When compared to the White COVID-19 hospitalization rate, the Black rate is 2.0 times higher and the Hispanic rate is 2.6 times higher. American Indians and Alaska Natives (AIAN) have the lowest hospitalization rate, at 0.6 times that of the White population, although racial misclassification is common for health outcomes of American Indians, which can lead to falsely lower rates.
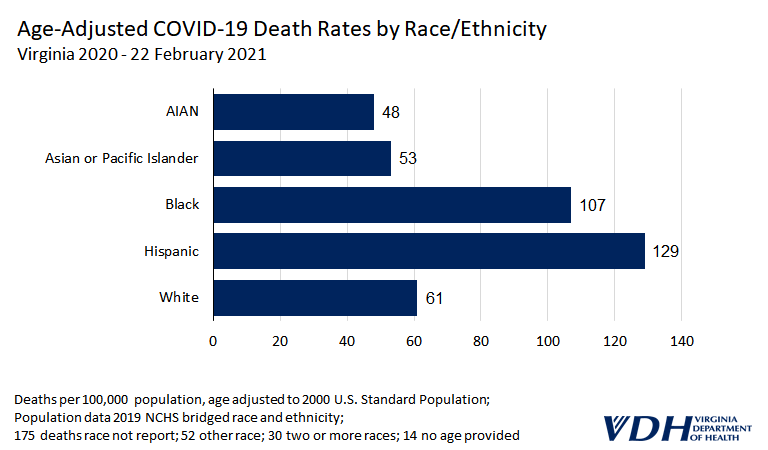
COVID-19 Deaths
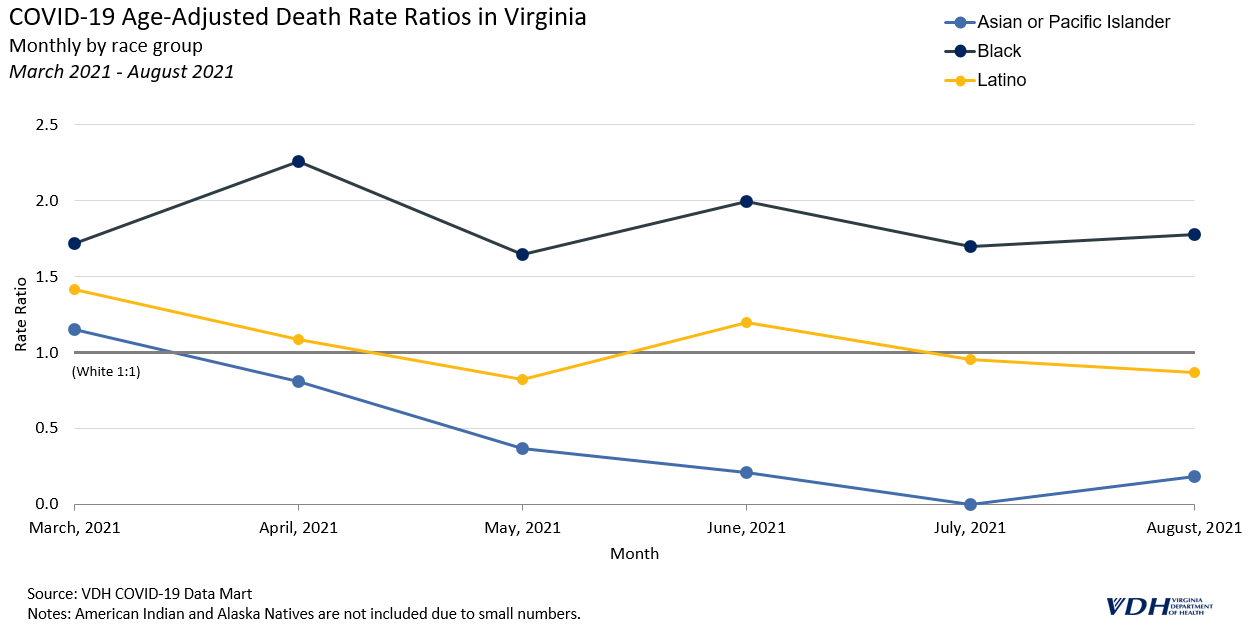
When comparing deaths among racial and ethnic groups, the analysis needs to account for the increased risk of death among older persons. For example, when comparing death rates of an older White population to a younger Hispanic population, age would be a contributing factor to any differences. One way to do this is to compare age group specific death rates for each racial/ethnic group. In Virginia, Hispanic and Black age-specific death rates are much higher than White age-specific death rates. The age group with the largest disparity was 35-44 year olds, with the Hispanic death rate 10.9 times higher and the Black rate 6.3 times higher than the White death rate. After this age group the size of the disparity steadily decreases. Among persons 85 years and older, the Hispanic rate is similar to the White rate, and the Black rate is 1.1 times higher than the White rate.
Another approach is to use age-adjusted rates. When compared to the White rate through February 22, 2021, the Hispanic age-adjusted COVID-19 death rate was 2.1 times higher; the Black rate was 1.8 times higher; the Asian rate was 0.9 times that of the White rate, and the American Indian/Alaska Native rate was 0.8 times that of the White rate. The disparities in death rates were worse earlier in the pandemic and decreased over time. When compared to the White rate through May 31, 2020, the Hispanic age-adjusted death rate was 3.5 times higher, the Black rate was 1.9 times higher, and the Asian rate was 1.8 times higher. In general, when compared to the White population, all other racial/ethnic groups’ age-adjusted death rates improved throughout the pandemic – even before vaccination was introduced. Hispanic to White population comparisons illustrate this most clearly. When compared to the White rate, the Hispanic rate was 3.5 times higher (May 31, 2020), then 3.1 times higher (September 30, 2020), then 2.4 times higher (December 22, 2020), and then 2.1 times higher (February 22, 2020).

COVID-19 Vaccinations
NOTE: The data in this section is outdated. Please refer to more recent posts for current data.
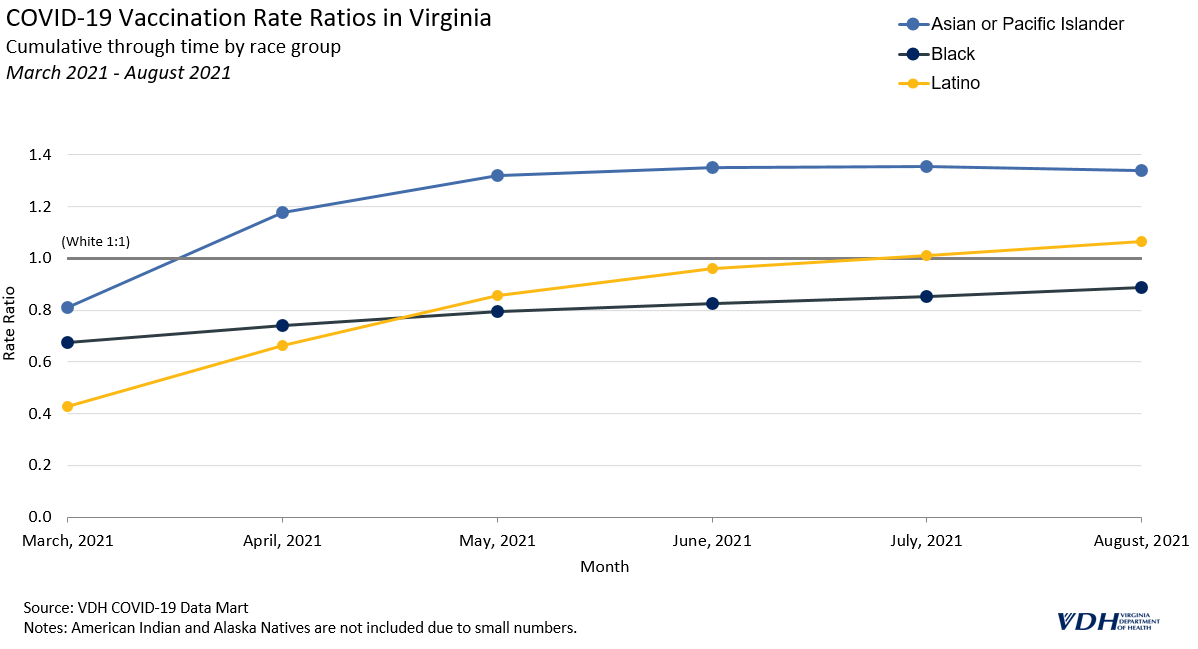
One of the key strategies to reduce disparities in infectious disease rates is vaccination. Ideally COVID-19 racial and ethnic disparities will lessen as the vaccination campaign in Virginia progresses. As of February 26, 2021, Black individuals had been vaccinated at a rate 0.6 times lower than White individuals. Hispanic and Asian/Pacific Islander individuals had even lower rates, at 0.5 times that of White individuals. When looking at only the 65 years and older population, which has been prioritized for vaccination, some of the vaccination rate disparities are smaller (Asian/Pacific Islander rate is 0.5 times lower than the White rate, Black rate is0.7 times lower and the Hispanic rate is 0.8 times lower.
Discussion
Opportunities for and threats to health in the United States and Virginia are distributed by race/ethnicity. The same exists during the COVID-19 pandemic. COVID-19 case, hospitalization and death rates are all greater for Black and Hispanic populations in Virginia. Differences in key social determinants of health, such as income, employment, and education contribute to these population-level disparities. More Hispanic adults in the United States reported stress about not having enough food (22.7%) or adequate housing (20.7%) than did White adults (11.9% and 9.2%, respectively). In addition, the risk of COVID-19 is increased for some racial/ethnic groups because they may be more likely to have less access to health care, reside in congregate living facilities and prisons, live in multigenerational families and hold jobs requiring in-person work (Gold, 2020). Additionally Black and Hispanic communities have higher rates of chronic health conditions, such as diabetes and high blood pressure, that are associated with complications and increased risk of death from COVID-19.
The United States and Virginia were overwhelmed by COVID-19 and particularly so at the beginning of the pandemic. Therefore it is not surprising that COVID-19 death disparities were greater at the beginning of the pandemic as groups at higher risk were more likely to be impacted. Unfortunately this also happens with other health problems as social determinants of health are maldistributed. These disparities will continue health problem by health problem until there is more equity in the distribution of social determinants of health across racial/ethnic groups.
Next Steps
It is critically important to continue to improve the tracking of racial and ethnic health and disease disparities. Since COVID-19 is the current major threat to health, this is a good place to work on improvements. The Virginia Department of Health (VDH) is prioritizing race and ethnicity as it upgrades its informatics systems in response to COVID-19, including ensuring race and ethnicity data are collected in a consistent manner across data systems, and that Hispanic ethnicity is presented alongside racial groups in the same tables and figures to allow for comparisons within Virginia and with other states. Additionally key interventions such as vaccination are being tracked by race and ethnicity to assure disparities are addressed.
VDH has worked to reduce missing data through communications, data matching, and requiring race and ethnicity fields when appropriate; however, missing race and ethnicity data continues to be an issue. While death records are mostly complete, the case, hospitalization, and vaccination data reported above still reflect significant amounts of missing data. VDH has adopted an imputation method to fill these gaps. More information using this method will be available in the coming weeks. The best way to protect the health of all Virginians is to reduce health disparities, ensuring we all prosper together.
References
Moore JT, Ricaldi JN, Rose CE, et al. (2020). Disparities in Incidence of COVID-19 Among Underrepresented Racial/Ethnic Groups in Counties Identified as Hotspots During June 5–18, 2020 — 22 States, February–June 2020. MMWR;69:1122–1126.
Gold JA, Rossen LM, Ahmad FB, et al. (2020) Race, Ethnicity, and Age Trends in Persons Who Died from COVID-19 — United States, May–August 2020. MMWR;69:1517–1521.
Painter EM, Ussery EN, Patel A, et al. (2021). Demographic Characteristics of Persons Vaccinated During the First Month of the COVID-19 Vaccination Program — United States, December 14, 2020–January 14, 2021. MMWR;70:174–177.
Lopez L, Hart LH, and Katz MH. (2021). Racial and Ethnic Health Disparities Related to COVID-19. JAMA;325(8):719-720. doi:10.1001/jama.2020.26443.
Andrasfay T and Goldman N (2021). Reductions in 2020 US life expectancy due to COVID-19 and the disproportionate impact on the Black and Latino populations. PNAS;118 (5) e2014746118; https://doi.org/10.1073/pnas.2014746118.
McKnight-Eily LR, Okoro CA, Strine TW, et al. (2021). Racial and Ethnic Disparities in the Prevalence of Stress and Worry, Mental Health Conditions, and Increased Substance Use Among Adults During the COVID-19 Pandemic — United States, April and May 2020. MMWR;70:162–166.