Last Updated: September 14, 2021
Vaccines are one of the greatest triumphs of medicine and public health. Polio, measles, rubella, and diphtheria, which once caused severe illness and death, have been eliminated in the United States thanks to comprehensive vaccination campaigns and routine childhood immunization programs. The virus that causes smallpox, which was once one of the most contagious and deadly diseases known, was eradicated through a global vaccination campaign and no longer exists in nature today. Vaccines combined with other public health efforts keep diseases like tetanus, yellow fever and rabies from circulating among people in the United States as well.
Highly effective vaccines are the best way to control outbreaks and prevent severe illness and death; however, no vaccine is 100 percent effective. As a result, it is important to study vaccine effectiveness to better understand how a vaccine can be used along with other public health mitigation measures to achieve optimum disease control.
In the early stages of a vaccination campaign, it is convenient to get a “snapshot” of how well a vaccine is working by looking at the number of cases of illness that occur among those who are fully vaccinated. This measure, however, is not a true measure of vaccine effectiveness. As the percentage of the population that is vaccinated (vaccine coverage) increases, the proportion of COVID-19 cases among vaccinated people increases. For example, during a 2006 mumps outbreak on a Virginia college campus, MMR (measles, mumps, rubella) vaccination was required for school entry and more than 99% of students were vaccinated. The vaccine effectiveness of the mumps component of the MMR vaccine is about 88%. A very small percentage of students developed mumps but all of the cases were vaccinated. The outbreak was quickly contained on campus and did not spill over to the community.
Vaccine effectiveness is calculated using carefully designed scientific studies that monitor the development of illness in groups of both vaccinated and unvaccinated people who are followed over a defined period of time. It is difficult to conduct a study of this complexity at a state level. However, it is possible to monitor how well the vaccine is working using a slightly different calculation that compares the attack rate (percentage of individuals who become ill) in those who are vaccinated (known as “breakthrough” infections) with the attack rate among the unvaccinated (“natural infections”).
Epidemiologists often use two by two (2×2) tables to make these calculations. The table below demonstrates how the attack rate is calculated for those who are vaccinated and those who are unvaccinated:
| Vaccinated | Unvaccinated | Total | |
|---|---|---|---|
| Infected | a | b | a+b |
| Not Infected | c | d | c+d |
| Total | a+c | b+d | a+b+c+d |
The attack rate among those who are vaccinated can be calculated as a/a+c and the attack rate among those who are unvaccinated can be calculated as b/b+d.
In order to determine vaccine effectiveness, epidemiologists make a calculation using the attack rates of both the vaccinated and unvaccinated groups. Vaccine effectiveness can be calculated as follows:
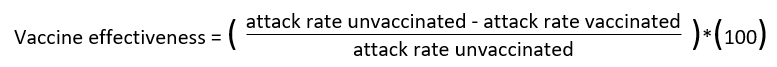
This vaccine effectiveness calculation returns a number that is between 0 and 100 and is interpreted as the proportionate reduction in disease among those who are vaccinated. A larger number indicates that a vaccine is more effective.
What do we know about the effectiveness of COVID-19 vaccines in the United States from published studies?
Currently, it appears that COVID-19 vaccines in the United States are highly effective at preventing serious illness and death and moderately to highly effective at preventing COVID-19 infection. A study released by the Centers for Disease Control and Prevention (CDC) on August 18, 2021, which followed fully vaccinated New York residents, found that current vaccines were highly effective (>90%) against hospitalization associated with COVID-19 and almost 80% effective against new infection, even when Delta variant was the prevalent circulating strain. In another study of U.S. nursing home residents, data showed that the effectiveness of COVID-19 vaccines against new infection declined from >70% to just over 50% once the Delta variant became the predominant circulating strain.
These data, as well as data from studies conducted in other countries, indicate that currently available COVID-19 vaccines in the United States remain highly protective against severe illness, hospitalization, and death due to COVID-19, but that protection against COVID-19 infection may be waning. VDH, in partnership with CDC, vaccine manufacturers, and other researchers will continue to monitor the vaccine effectiveness of COVID-19 vaccines. Vaccine effectiveness, along with other epidemiologic data, can equip public health policymakers with the necessary tools needed to make sound decisions about vaccination and mitigation strategies to help reduce the burden of COVID-19 in the United States and around the world.
One such example is the recent White House’s announcement about plans to provide booster doses to adults who have received the mRNA COVID-19 series if the Food and Drug Administration (FDA) and the Advisory Committee on Immunization Practices (ACIP) recommend them this fall. More information about Virginia’s plan for vaccine booster doses and additional data on vaccine effectiveness will be available in the coming weeks.