Last Updated: June 4, 2021
by Michael Landen & Rexford Anson-Dwamena
COVID-19 Death Disparities by Census Tract Poverty Level, Health Opportunity Index and Rurality
Disparities for key COVID-19 indicators by race/ethnicity in Virginia and the United States have been well documented (see March 8, 2021 COVID-19 Health and Disease Disparities by Race and Ethnicity in Virginia blog post). This report focuses on COVID-19 death rate disparities for adults 35-54 years of age in Virginia by census tract level poverty, health opportunity index and rurality. The entire age range was not used for this analysis because subpopulations, such as those with different poverty levels, have different age structures and therefore can’t be fairly compared for an outcome that is associated with age such as COVID-19 death. The 35-54 year age group was chosen for these comparisons because it is the youngest age group with sufficient numbers of deaths to allow for reasonable death rate comparisons at the census tract level.
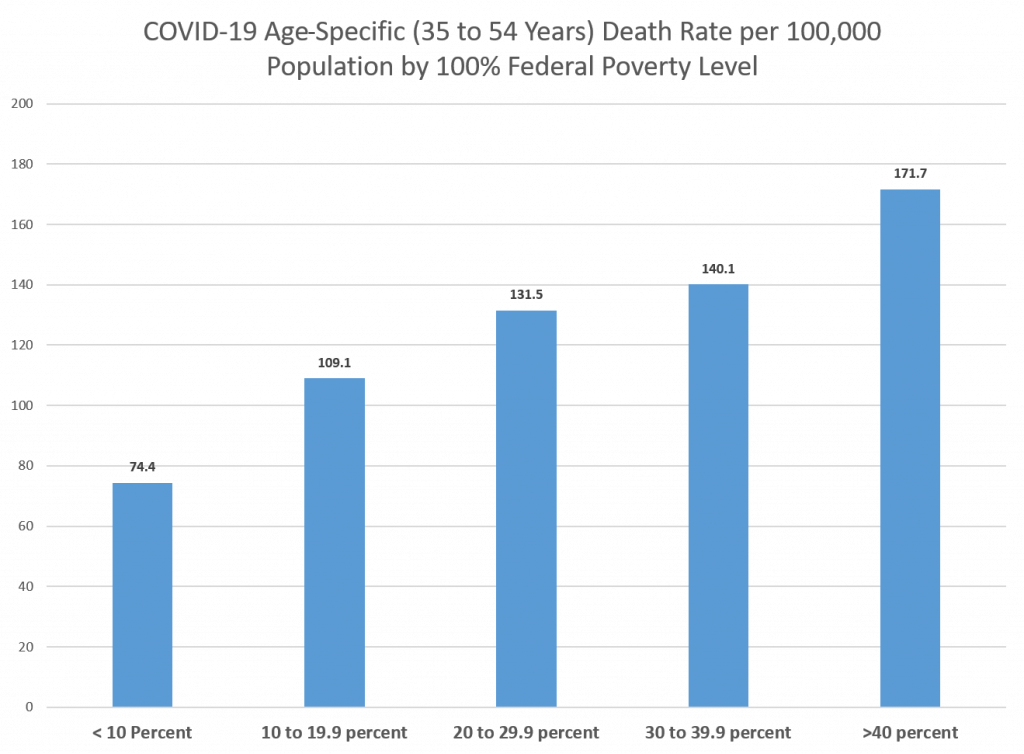
Poverty Level Disparities
A person’s income is not included in their death records, however, the percentage of persons living below the federal poverty level by census tract is available. COVID-19 deaths among persons 35-54 years of age can be grouped by this percentage. The largest disparity in the COVID-19 death rate was found between those living in census tracts with the greatest percentage of persons living in poverty, >= 40%, and those living in census tracts with the lowest percentage of persons living in poverty, < 10%. Persons living in census tracts with the highest percentage of people in poverty were 2.3 times more likely to die of COVID-19 than those from the lowest poverty census tracts (Figure 1).
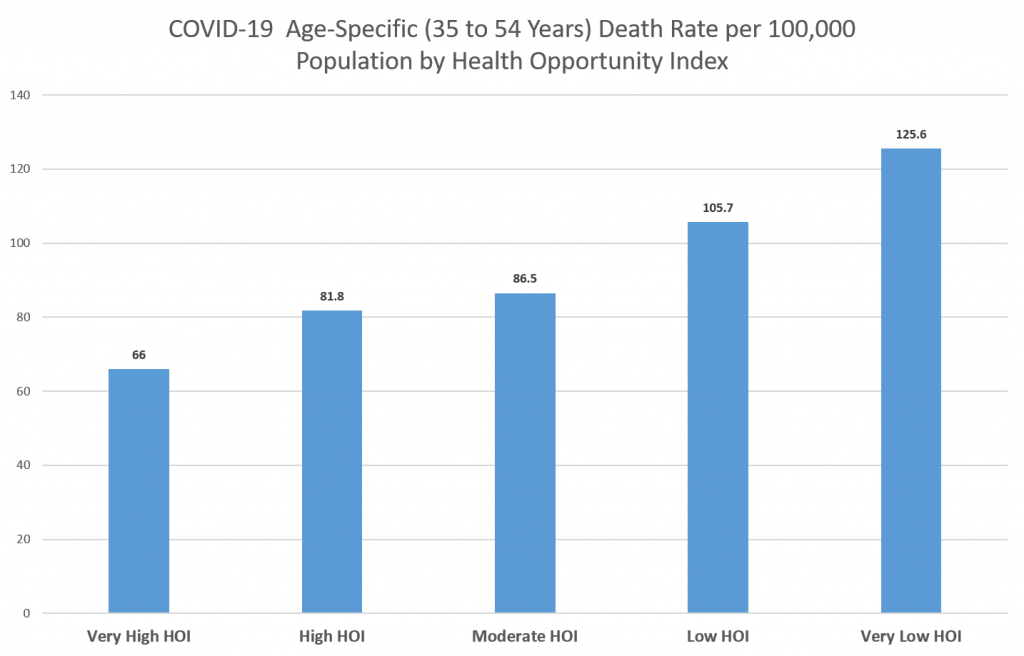
Health Opportunity Index Disparities
The Virginia Department of Health provides the Virginia Health Opportunity Index (HOI) which is a composite measure of the social determinants of health – the social, economic, educational and environmental factors that relate to a community’s well-being – at the census tract level. The index is divided into 5 levels – very high, high, moderate, low, and very low – and census tracts can be grouped into these 5 levels. In general, persons living in census tracts with a higher HOI tend to have lower disease and death rates. COVID-19 deaths among persons 35-54 years of age can be grouped by the level of HOI for the census tract in which they reside. The largest disparity in the COVID-19 death rate for this age group was found between those living in census tracts with the lowest HOI and those living in census tracts with the highest HOI. Persons living in census tracts with the lowest HOI were 1.9 times more likely to die of COVID-19 than those from census tracts with the highest HOI (Figure 2).
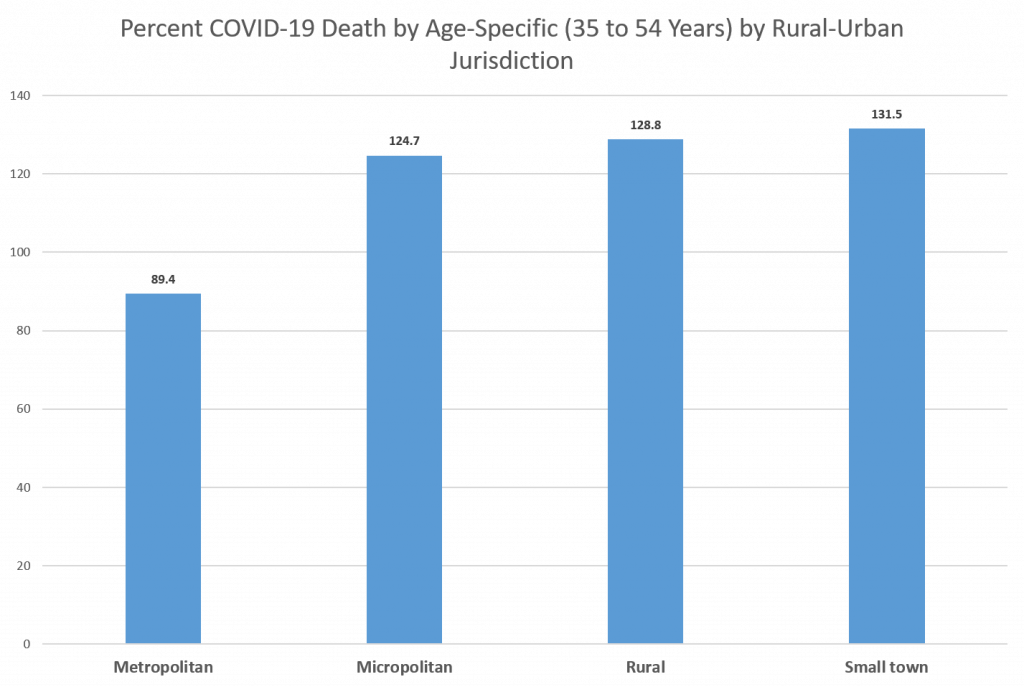
Rurality Disparities
Persons living in rural areas, in general, tend to have higher disease and death rates than those living in metropolitan areas. Rural and urban census tracts can be classified by the Rural/Urban Community Area (RUCA) taxonomy and then further classified into groups – metropolitan, micropolitan, small town and rural. COVID-19 deaths among persons 35-54 years of age can be grouped by these RUCA groups for the census tract in which they resided. The largest disparity in the COVID-19 death rate for this age group was found between those living in small town census tracts and those living in metropolitan census tracts. Persons living in small town census tracts were 1.5 times more likely to die of COVID-19 than those from metropolitan census tracts, and both persons from micropolitan census tracts and persons from rural census tracts were 1.4 times more likely to die of COVID-19 than those from metropolitan census tracts (Figure 3).
COVID-19 death rates for those 35-54 years are higher in non-metropolitan communities and for persons living in communities with a higher percentage of people living in poverty in Virginia. This is not surprising since many health indicators are worse for communities with high poverty rates and for rural communities. In general, these communities may have fewer opportunities than communities with lower poverty and metropolitan communities. One approach to reducing these disparities is to increase social, economic, vocational and educational opportunities in these high poverty communities and rural communities. An “opportunity” specifically related to COVID-19 is vaccination, and these vaccinations should continue to be prioritized for persons in rural communities and those with high poverty rates or percentages.

